Gram negative cocci
Gram negative cocci :
Gram-negative cocci are spherical bacteria that do not retain the crystal violet stain used in the Gram staining procedure, appearing pink after being counterstained. Key examples include:
Neisseria: This genus includes Neisseria gonorrhoeae, the causative agent of gonorrhea, and Neisseria meningitidis, which can cause meningococcal meningitis. Moraxella :Moraxella catarrhalis is often associated with respiratory infections.
These bacteria are known for their pathogenic potential and are typically studied in clinical microbiology for diagnosis and treatment of infections.
Neisseria gonorrhoeae is a bacterium that causes the sexually transmitted infection gonorrhea. It's a gram-negative diplococcus and primarily infects the mucous membranes of the urogenital tract, but can also affect the throat and rectum.
Key Points:
Transmission:Primarily through sexual contact, including vaginal, anal, and oral sex.
Symptoms: In men, symptoms may include painful urination, pus discharge from the penis, and swollen testicles. Women may experience increased vaginal discharge, painful urination, and pelvic pain, though many women are asymptomatic.
Complications: If untreated, gonorrhea can lead to serious health issues, including pelvic inflammatory disease (PID) in women, infertility, and an increased risk of HIV.
Diagnosis: Typically diagnosed through urine tests or swabs from the affected area.
Treatment: Gonorrhea is treated with antibiotics, although resistance is becoming a significant issue.
Regular testing and safe sex practices can help prevent the spread of gonorrhea and other STIs.
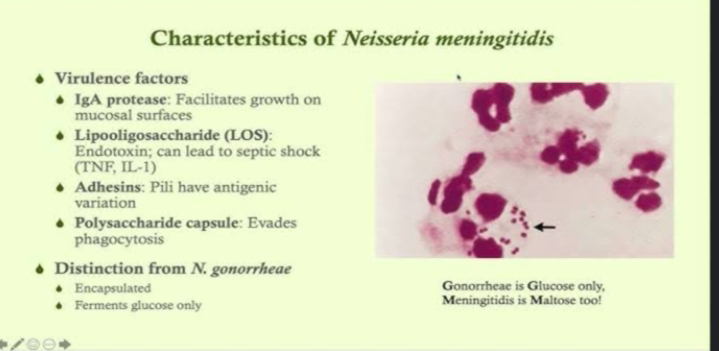
Neisseria meningitis :
Neisseria meningitidis, commonly known as meningococcus, is a bacterium that can cause meningitis and other serious infections. It is typically found in the throat and can be spread through respiratory droplets. Meningococcal disease can lead to meningitis, which is inflammation of the protective membranes covering the brain and spinal cord, and septicemia, a life-threatening infection of the bloodstream.
Key Points:
Transmission: Spread through close contact, such as kissing or sharing utensils.
Symptoms: Sudden onset of fever, headache, stiff neck, nausea, vomiting, sensitivity to light, and altered mental status.
Diagnosis: Usually confirmed through blood cultures or cerebrospinal fluid analysis.
Treatment: Prompt antibiotic therapy is crucial. Common antibiotics include penicillin and ceftriaxone.
Prevention: Vaccination is available and recommended, particularly for adolescents and those in close living quarters, like college dorms.
Types of Vaccines:
1.Meningococcal conjugate vaccines (MenACWY)
2.Serogroup B vaccines (MenB)
Meningococcus can cause meningitis and other forms of meningococcal disease. It initially produces general symptoms like fatigue, fever, and headache and can rapidly progress to neck stiffness, coma and death in 10% of cases. Petechiae occur in about 50% of cases. Chance of survival is highly correlated with blood cortisol levels, with lower levels prior to steroid administration corresponding with increased patient mortalitySymptoms of meningococcal meningitis are easily confused with those caused by other bacteria, such as Haemophilus influenzae and Streptococcus pneumoniae Suspicion of meningitis is a medical emergency and immediate medical assessment is recommended. Current guidance in the United Kingdom is that if a case of meningococcal meningitis or septicaemia (infection of the blood) is suspected, intravenous antibiotics should be given and the ill person admitted to the hospital. This means that laboratory tests may be less likely to confirm the presence of Neisseria meningitidis as the antibiotics will dramatically lower the number of bacteria in the body. The UK guidance is based on the idea that the reduced ability to identify the bacteria is outweighed by reduced chance of death.[citation needed]
Septicaemia caused by Neisseria meningitidis has received much less public attention than meningococcal meningitis even though septicaemia has been linked to infant deaths. Meningococcal septicaemia typically causes a purpuric rash, that does not lose its color when pressed with a glass slide ("non-blanching") and does not cause the classical symptoms of meningitis. This means the condition may be ignored by those not aware of the significance of the rash. Septicaemia carries an approximate 50% mortality rate over a few hours from initial onset.[citation needed]
Other severe complications include Waterhouse–Friderichsen syndrome, a massive, usually bilateral, hemorrhage into the adrenal glands caused by fulminant meningococcemia, adrenal insufficiency, and disseminated intravascular coagulation.
Not all instances of a purpura-like rash are due to meningococcal septicaemia; other possible causes, such as idiopathic thrombocytopenic purpura (ITP; a platelet disorder) and Henoch–Schönlein purpura, also need prompt investigation.[citation needed]
Gram-Negative Bacteria :
Like Gram-positive bacteria, Gram-negative organisms can be cocci or rods. Most Gram-negative bacteria are rods, but a few important species are in cocci form. Neisseria species are Gram-negative cocci that typically attach in pairs and are some of the most common aerobic Gram-negative cocci. Neisseria meningitidis is a common cause of meningitis in children and young adults. Neisseria gonorrheae is an important cause of urethritis and cervicitis.
Most of the Gram-negative infections encountered involve aerobic rod species, though two key anaerobic species are worth mentioning: Fusobacterium and Bacteroides. Fusobacterium is a filamentous Gram-negative rod typically found in the oropharynx that can cause severe head and neck infections—specifically, Lemierre syndrome. Bacteroides, in contrast, is typically found in the GI tract below the diaphragm and is often implicated in intraabdominal abscesses, diverticulitis, and GI tract infections.
Of the aerobic Gram-negative rods, lactose fermentation is evaluated on MacConkey agar. This selective indicator agar turns pink in the presence of a colony that ferments lactose and remains yellow for those that do not ferment lactose. Key lactose fermenters include Escherichia coli, Klebsiella, and Enterobacter.